
Difference Between Symptoms of Hyperglycemia and Hypoglycemia
Table of Contents
ToggleIntroduction to the symptoms of hyperglycemia and hypoglycemia and its impact on the body
When it comes to understanding my health, I’ve realized that blood sugar levels play a pivotal role in the overall functioning of my body. What is blood sugar, you may ask? Essentially, it represents the concentration of glucose present in my bloodstream at any given time. Glucose, a simple sugar, serves as a primary energy source for my cells, and its balance is critical for maintaining the energy required for bodily functions.
However, the concentration of glucose in my blood isn’t constant; it fluctuates throughout the day. These changes are influenced by factors such as the meals I consume, the level of physical activity I engage in, and how my body manages insulin. Insulin is the hormone responsible for helping my cells absorb glucose and use it for energy, and any disruption in its function can lead to blood sugar imbalances.
The two extremes of blood sugar levels – hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) – can have profound and sometimes dangerous impacts on my body. They can influence my energy levels, mood, and even my long-term health, leading to complications if left unmanaged. Understanding these conditions and their differences is essential for maintaining optimal health and preventing potential health issues.

What are the symptoms of hyperglycemia?
Hyperglycemia occurs when there’s an excess amount of glucose circulating in my bloodstream. It usually manifests when my body has insufficient insulin or when it cannot effectively use the insulin it has. This can be a temporary condition, often resulting from dietary choices, or it may be chronic, as seen in diabetes mellitus.
Difference Between Symptoms of Hyperglycemia and Hypoglycemia
Hyperglycemia refers to elevated levels of glucose (sugar) in the blood and is commonly associated with diabetes. Symptoms of hyperglycemia can develop gradually and may vary from person to person. Common signs include:
- Increased Thirst (Polydipsia): Feeling unusually thirsty despite drinking fluids.
- Frequent Urination (Polyuria): Needing to urinate more often than usual, especially during the night.
- Fatigue: Experiencing unusual tiredness or weakness.
- Blurred Vision: Difficulty focusing or seeing clearly.
- Headaches: Persistent or frequent headaches.
- Dry Mouth: A constant feeling of dryness in the mouth.
- Unintended Weight Loss: Losing weight without changes in diet or exercise.
- Slow-Healing Wounds: Cuts or sores that take longer than usual to heal.
- Recurrent Infections: Such as skin, gum, or vaginal infections.
- Difficulty Concentrating: Trouble focusing or feeling mentally sluggish.
- Nausea or Vomiting: Feeling sick to the stomach, which can be a sign of severe hyperglycemia.
In more severe cases, extremely high blood sugar levels can lead to conditions like diabetic ketoacidosis (DKA) in type 1 diabetes or hyperosmolar hyperglycemic state (HHS) in type 2 diabetes. These conditions are medical emergencies characterized by:
- Abdominal Pain
- Rapid Breathing
- Fruity-Smelling Breath
- Confusion or Loss of Consciousness
If you or someone else is experiencing symptoms of hyperglycemia, especially severe ones, it’s important to seek medical attention promptly. Early intervention can help manage blood sugar levels effectively and prevent complications.
Causes of Symptoms of hyperglycemia
Causes of Hyperglycemia
- Diabetes Mellitus:
- Type 1 Diabetes: An autoimmune disorder where the pancreas produces little or no insulin due to the destruction of insulin-producing beta cells.
- Type 2 Diabetes: Characterized by insulin resistance, where the body’s cells do not respond properly to insulin, and often accompanied by a relative lack of insulin production.
- Gestational Diabetes:
- Occurs during pregnancy when hormonal changes make cells less responsive to insulin.
- Medications:
- Certain drugs can elevate blood glucose levels, including corticosteroids, beta-blockers, diuretics, and some antipsychotics.
- Hormonal Disorders:
- Conditions like Cushing’s syndrome (excess cortisol production) or acromegaly (excess growth hormone) can interfere with insulin action.
- Pancreatic Diseases:
- Disorders like pancreatitis or pancreatic cancer that affect insulin production.
- Stress and Illness:
- Physical stress from surgery, trauma, or infections can increase stress hormones like cortisol and adrenaline, leading to elevated blood sugar levels.
- Genetic Factors:
- Rare genetic mutations affecting insulin production or utilization.
- Dietary Choices:
- Consuming excessive carbohydrates without adequate insulin response can raise blood glucose levels.
- Sedentary Lifestyle:
- Lack of physical activity can contribute to insulin resistance.

Causes of Symptoms of hyperglycemia
Symptoms of Hyperglycemia
Early recognition of hyperglycemia symptoms can prevent complications:
- Increased Thirst (Polydipsia):
- High blood sugar levels cause dehydration, prompting increased fluid intake.
- Frequent Urination (Polyuria):
- The kidneys excrete excess glucose, leading to increased urine production.
- Blurred Vision:
- Elevated glucose levels can cause swelling in the eye lenses.
- Fatigue:
- Inability of cells to absorb glucose leads to a lack of energy.
- Headaches:
- Resulting from dehydration and high blood sugar levels.
- Dry Mouth and Skin:
- Due to fluid loss through increased urination.
- Slow-Healing Wounds or Frequent Infections:
- High glucose impairs immune function and circulation.
- Unexplained Weight Loss:
- The body breaks down fat and muscle for energy when it can’t utilize glucose.
- Nausea and Vomiting:
- Can occur if hyperglycemia progresses to diabetic ketoacidosis (more common in Type 1 diabetes).
- Fruity-Smelling Breath:
- Indicates the presence of ketones, a byproduct of fat metabolism.
- Difficulty Concentrating:
- Fluctuations in blood sugar can affect cognitive functions.
When to Seek Medical Attention
If you experience symptoms of hyperglycemia, especially with risk factors for diabetes, consult a healthcare provider promptly. Untreated hyperglycemia can lead to serious complications:
- Diabetic Ketoacidosis (DKA):
- A life-threatening condition from extremely high glucose levels and ketone buildup, primarily in Type 1 diabetes.
- Hyperosmolar Hyperglycemic State (HHS):
- Severe dehydration and high blood sugar levels, more common in Type 2 diabetes.
Prevention and Management
- Regular Monitoring:
- Frequent blood glucose testing to manage and adjust treatment plans.
- Medications:
- Use insulin therapy or oral hypoglycemic agents as prescribed.
- Healthy Diet:
- Balance carbohydrate intake with proteins and healthy fats; follow a meal plan recommended by a dietitian.
- Physical Activity:
- Engage in regular exercise to improve insulin sensitivity.
- Hydration:
- Drink plenty of water to help kidneys eliminate excess glucose.
- Stress Management:
- Techniques like meditation, yoga, or deep-breathing exercises can help regulate blood sugar levels.
- Education:
- Learn about diabetes management to make informed decisions about your health.
Early detection and management of hyperglycemia are vital to prevent long-term complications such as cardiovascular disease, nerve damage, kidney failure, and vision problems. Regular check-ups and adherence to treatment plans can significantly improve quality of life.
Risks and Complications of Hyperglycemia
If I consistently experience high blood sugar levels, the risks and complications associated with hyperglycemia can be severe. Over time, chronic hyperglycemia can damage blood vessels and nerves, leading to a spectrum of complications that affect almost every part of my body.

Risks and Complications of Hyperglycemia
Acute Complications
- Diabetic Ketoacidosis (DKA):
- Description: A serious condition where the body starts breaking down fats at an excessive rate, producing ketones, which makes the blood acidic.
- Symptoms: Frequent urination, excessive thirst, nausea, abdominal pain, shortness of breath, fruity-scented breath.
- Risk: Primarily affects people with type 1 diabetes but can occur in type 2.
- Hyperosmolar Hyperglycemic State (HHS):
- Description: Extremely high blood sugar levels without significant ketone production, leading to severe dehydration.
- Symptoms: High blood glucose levels, dry mouth, extreme thirst, warm skin without sweating, fever, confusion, vision loss.
- Risk: More common in older adults with type 2 diabetes.
Chronic Complications
- Cardiovascular Disease:
- Risks: Increased likelihood of coronary artery disease, heart attack, stroke, atherosclerosis (narrowing of arteries), and hypertension.
- Cause: High glucose levels damage blood vessels and nerves controlling the heart.
- Neuropathy (Nerve Damage):
- Peripheral Neuropathy: Causes tingling, pain, numbness in hands and feet.
- Autonomic Neuropathy: Affects digestive system, urinary tract, sexual organs, leading to issues like gastroparesis, bladder problems, erectile dysfunction.
- Nephropathy (Kidney Damage):
- Risks: Can progress to kidney failure or end-stage renal disease requiring dialysis or transplantation.
- Cause: Damage to the blood vessel clusters in kidneys that filter waste.
- Retinopathy (Eye Damage):
- Risks: Vision problems, including blindness.
- Conditions: Diabetic retinopathy, cataracts, glaucoma.
- Cause: Damage to blood vessels in the retina.
- Foot Damage:
- Risks: Foot ulcers, infections, and possible amputations.
- Cause: Poor blood flow and nerve damage reduce sensation and healing ability.
- Skin Conditions:
- Risks: Bacterial and fungal infections, itching.
- Conditions: Diabetic dermopathy, necrobiosis lipoidica diabeticorum.
- Hearing Impairment:
- Risks: Higher likelihood of hearing problems.
- Cause: Damage to nerves and blood vessels in the ear.
- Alzheimer’s Disease:
- Risks: Potentially higher risk of cognitive decline and Alzheimer’s.
- Cause: Links between insulin resistance and brain function are being studied.
- Bone and Joint Disorders:
- Risks: Conditions like osteoporosis, Charcot joint.
- Cause: Nerve damage and poor blood flow weaken bones and joints.
Other Health Issues
- Gum Disease:
- Risks: Infections in the gums and bones that hold teeth in place.
- Cause: High glucose levels promote bacterial growth in the mouth.
- Depression:
- Risks: Mental health challenges are more common, affecting diabetes management.
- Cause: The stress of managing a chronic condition.
- Compromised Immune System:
- Risks: Increased susceptibility to infections.
- Cause: High glucose impairs white blood cell function.
Preventive Measures
- Blood Sugar Monitoring: Regular checks to maintain target glucose levels.
- Medication Adherence: Taking insulin or oral medications as prescribed.
- Healthy Diet: Emphasizing fiber, whole grains, fruits, and vegetables.
- Physical Activity: Regular exercise to improve insulin sensitivity.
- Regular Check-ups: Eye exams, foot exams, and screenings for kidney function.
- Smoking Cessation: Smoking exacerbates cardiovascular and circulatory issues.
- Stress Management: Techniques like mindfulness can improve blood sugar control.
Hyperglycemia poses significant health risks that can impact quality of life and longevity. Early detection and proactive management are vital. Individuals should work closely with healthcare providers to develop personalized plans that address blood sugar control and monitor for potential complications.
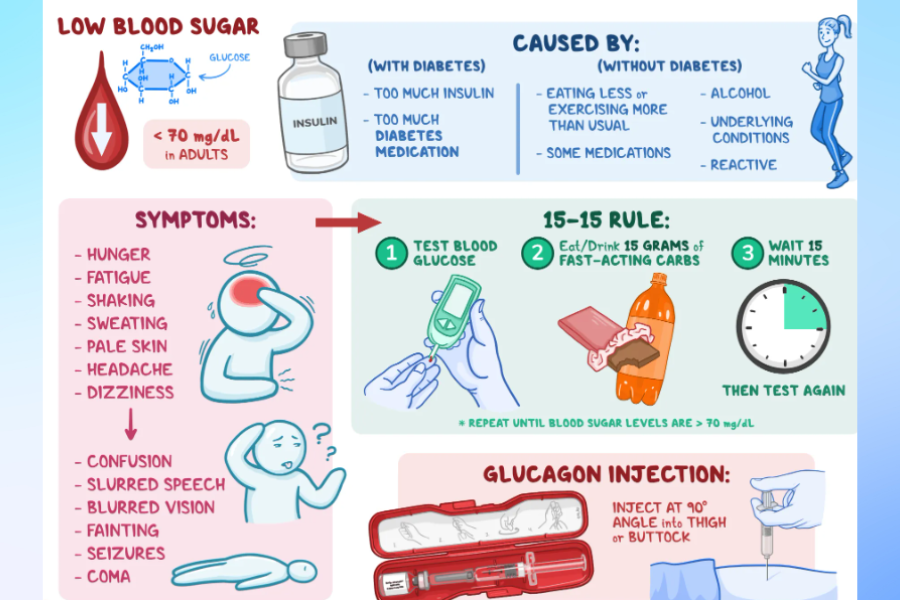
What are the symptoms of hypoglycemia?
Hypoglycemia, or low blood sugar, occurs when the glucose levels in your blood drop below normal. This condition is most commonly associated with diabetes treatment but can also happen due to other medical conditions or prolonged fasting. Recognizing the symptoms early is crucial to prevent severe complications.

What are the symptoms of hypoglycemia?
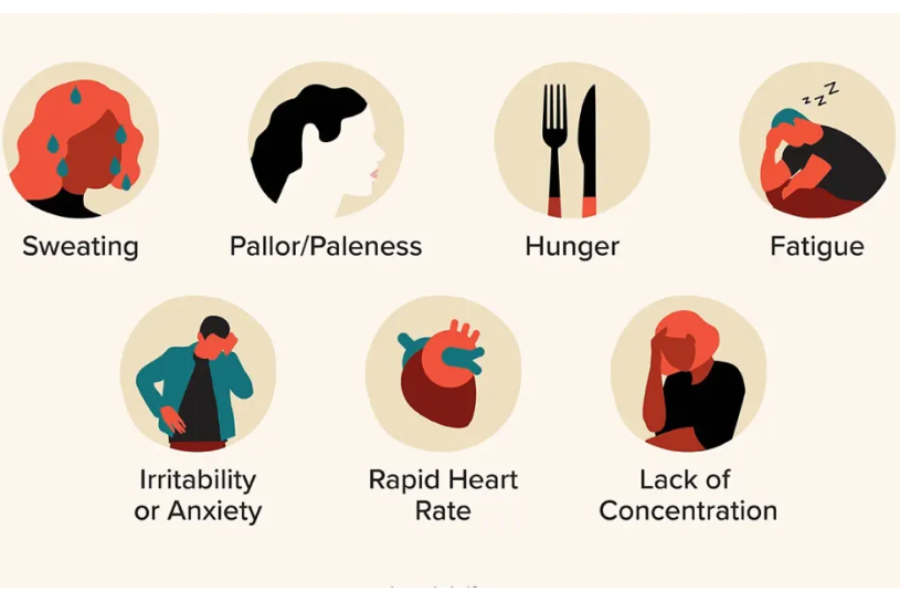
Common Symptoms of Hypoglycemia
- Shakiness or Trembling: Feeling jittery or experiencing tremors in your hands.
- Sweating: Sudden onset of perspiration, especially without physical exertion.
- Hunger: Intense feelings of hunger, even after eating.
- Dizziness or Lightheadedness: Feeling faint or unsteady.
- Heart Palpitations: Rapid or irregular heartbeat.
- Anxiety or Nervousness: Unexplained feelings of unease or agitation.
- Irritability or Mood Changes: Sudden shifts in mood or unexplained irritability.
- Headaches: Onset of dull or throbbing headaches.
- Blurred Vision: Difficulty focusing or seeing clearly.
- Fatigue or Weakness: Feeling unusually tired or lacking energy.
Severe Symptoms
If hypoglycemia is not addressed promptly, more serious symptoms may develop:
- Confusion or Difficulty Concentrating: Trouble thinking clearly or making decisions.
- Slurred Speech: Difficulty articulating words.
- Loss of Coordination: Trouble walking or performing simple tasks.
- Seizures: Uncontrolled muscle contractions.
- Loss of Consciousness: Fainting or inability to awaken.
What to Do If You Experience Symptoms
- Check Blood Sugar Levels: If you have a glucose meter, test your blood sugar immediately.
- Consume Fast-Acting Carbohydrates: Eat or drink something with 15-20 grams of glucose or simple carbs, such as glucose tablets, fruit juice, or regular (not diet) soda.
- Recheck After 15 Minutes: Test your blood sugar again to see if it has improved.
- Seek Medical Attention: If symptoms persist or worsen, contact a healthcare professional immediately.
When to Consult a Doctor
- Frequent Episodes: Regular occurrences of hypoglycemia require medical evaluation.
- Unknown Cause: If you experience symptoms without a known reason, seek medical advice.
- Medication Adjustment: If you’re diabetic, your treatment plan may need modification.
Hypoglycemia can be a sign of an underlying health issue. It’s important to consult a healthcare provider for a proper diagnosis and personalized guidance.
What causes hypoglycemia?
Hypoglycemia occurs when blood sugar (glucose) levels drop below normal. Glucose is the body’s main source of energy, and low levels can affect bodily functions. The causes of hypoglycemia can vary depending on whether a person has diabetes or not.

Difference Between Symptoms of Hyperglycemia and Hypoglycemia
In People with Diabetes:
- Medication Overdose:
- Insulin Overuse: Taking too much insulin is a common cause. This might happen if the dosage is miscalculated or injected incorrectly.
- Oral Diabetes Medications: Some medications, like sulfonylureas and meglitinides, stimulate insulin production and can cause hypoglycemia if not properly dosed.
- Skipping or Delaying Meals:
- Eating less than usual or missing a meal can lead to low blood sugar, especially after taking diabetes medications.
- Increased Physical Activity:
- Exercise uses glucose for energy. If activity levels increase without adjusting food intake or medication, blood sugar can drop.
- Alcohol Consumption:
- Drinking alcohol, particularly on an empty stomach, can interfere with the liver’s ability to release glucose.
In People Without Diabetes:
- Medications:
- Certain drugs like quinine, some antibiotics, and beta-blockers can cause hypoglycemia.
- Excessive Alcohol Intake:
- Heavy drinking without eating can prevent the liver from releasing stored glucose.
- Critical Illnesses:
- Liver Diseases: Conditions like hepatitis can impair glucose production.
- Kidney Disorders: Reduced kidney function can affect medication clearance, leading to hypoglycemia.
- Severe Infections: The body’s response to infection can alter glucose metabolism.
- Hormonal Deficiencies:
- Adrenal Insufficiency: Low cortisol levels can decrease glucose production.
- Pituitary Disorders: These can affect hormones that regulate glucose.
- Insulin Overproduction:
- Insulinomas: Rare pancreatic tumors produce excess insulin.
- Non-Insulinoma Pancreatogenous Hypoglycemia Syndrome (NIPHS): A condition causing overproduction of insulin.
- Reactive Hypoglycemia:
- Occurs within a few hours after eating due to excessive insulin release.
- Starvation and Eating Disorders:
- Prolonged fasting or conditions like anorexia nervosa reduce glucose availability.
- Enzyme Deficiencies:
- Genetic conditions affecting carbohydrate metabolism can cause hypoglycemia, especially in infants and children.
Other Contributing Factors:
- Strenuous Exercise: Even in non-diabetics, intense physical activity without adequate nutrition can lower blood sugar.
- Pregnancy: Hormonal changes can affect glucose levels.
- Age: Infants and the elderly are more susceptible due to metabolic differences.
Hypoglycemia results from an imbalance between glucose intake, production, and utilization. It’s essential to identify the underlying cause to manage and prevent future episodes effectively. If experiencing symptoms like shakiness, dizziness, sweating, or confusion, it’s important to seek medical attention.
What are the risks and complications of hypoglycemia?
Hypoglycemia occurs when blood glucose levels fall below normal, typically below 70 mg/dL (3.9 mmol/L). While it is most commonly associated with diabetes treatment, it can also occur in individuals without diabetes due to various conditions or factors. The risks and complications of hypoglycemia can be immediate (acute) or long-term, affecting multiple body systems and overall quality of life.
What are the risks and complications of hypoglycemia
Immediate (Acute) Risks and Complications
- Neurological Symptoms:
- Cognitive Impairment: Confusion, difficulty concentrating, and poor judgment can occur due to insufficient glucose supply to the brain.
- Physical Weakness: Fatigue, dizziness, and lack of coordination may lead to falls or injuries.
- Visual Disturbances: Blurred or double vision can impair daily activities.
- Autonomic Symptoms:
- Adrenergic Responses: Shakiness, palpitations, and anxiety result from the body’s release of adrenaline.
- Cholinergic Responses: Sweating, hunger, and tingling sensations are common signs.
- Severe Hypoglycemia:
- Seizures: Prolonged low blood sugar can trigger convulsions.
- Loss of Consciousness: Fainting or slipping into a coma is possible if hypoglycemia is not promptly treated.
- Death: In extreme cases, especially if untreated, hypoglycemia can be fatal.
- Accidents and Injuries:
- Motor Vehicle Accidents: Hypoglycemia can impair driving ability, increasing the risk of accidents.
- Workplace Hazards: Operating machinery or performing tasks requiring alertness becomes dangerous.
Long-Term Risks and Complications
- Hypoglycemia Unawareness:
- Blunted Symptoms: Repeated episodes can reduce the body’s warning signs, making future hypoglycemic events harder to detect.
- Increased Severity: Lack of awareness can lead to more severe and sudden hypoglycemic episodes.
- Cardiovascular Issues:
- Arrhythmias: Low blood sugar can cause irregular heartbeats.
- Cardiac Events: There’s an increased risk of angina or myocardial infarction due to stress on the heart.
- Neurological Damage:
- Cognitive Decline: Chronic hypoglycemia may contribute to long-term memory problems and decreased mental function.
- Developmental Delays in Children: Severe episodes can affect brain development in infants and young children.
- Psychological Impact:
- Anxiety and Depression: Fear of hypoglycemic episodes can lead to mental health issues.
- Social Isolation: Symptoms may cause individuals to withdraw from social activities.
- Poor Glycemic Control:
- Overcompensation: Fear of low blood sugar may lead individuals to keep their glucose levels too high, increasing the risk of hyperglycemia and its associated complications.
- Economic Burden:
- Medical Costs: Frequent hospitalizations and treatments add financial strain.
- Reduced Productivity: Time off work and decreased performance can impact income and career progression.
Additional Considerations
- Impact on Quality of Life: The constant monitoring and management can be stressful and overwhelming.
- Interference with Daily Activities: Regular tasks become challenging due to the need to manage symptoms and prevent episodes.
- Strain on Relationships: Mood swings and behavioral changes can affect family and social dynamics.
Prevention and Management Strategies
- Regular Monitoring: Frequent blood glucose checks help in early detection and management.
- Education: Understanding symptoms and treatment options empowers individuals to take prompt action.
- Medication Management: Adjusting insulin or other glucose-lowering medications under medical supervision can reduce risks.
- Diet and Nutrition: Balanced meals and regular eating schedules help maintain stable blood sugar levels.
- Emergency Planning: Keeping fast-acting carbohydrates on hand and informing others about how to assist during an episode is crucial.
It’s important to work closely with healthcare professionals to manage hypoglycemia effectively and mitigate its risks and complications.
Key Differences Between Symptoms of Hyperglycemia and Hypoglycemia
While both hyperglycemia and hypoglycemia concern blood sugar levels, their symptoms differ significantly, reflecting the contrasting effects of excess and insufficient blood glucose. One of the key differences is the speed at which they develop. Hypoglycemia symptoms can arise quickly and require immediate attention, whereas hyperglycemia symptoms tend to develop more slowly and may go unnoticed initially.
Difference Between Symptoms of Hyperglycemia and Hypoglycemia
Hyperglycemia (High Blood Sugar)
Common Symptoms:
- Increased Thirst and Dry Mouth: Elevated glucose levels cause the body to draw fluid from tissues, leading to dehydration.
- Frequent Urination: The kidneys work overtime to eliminate excess sugar, resulting in more frequent urination.
- Blurred Vision: High sugar levels can cause the lenses in the eyes to swell.
- Fatigue: The body’s inability to utilize glucose efficiently leads to energy depletion.
- Headaches: Dehydration and high glucose levels can trigger headaches.
- Unintended Weight Loss: Despite eating normally, the body cannot absorb glucose properly, leading to weight loss.
- Slow-Healing Sores or Frequent Infections: High sugar levels can impair circulation and the immune system.
Onset and Progression:
- Gradual Development: Symptoms often develop slowly over days or weeks.
- Severity: If left unmanaged, hyperglycemia can lead to serious complications like diabetic ketoacidosis.
Hypoglycemia (Low Blood Sugar)
Common Symptoms:
- Shakiness or Trembling: The body’s response to low glucose triggers adrenaline release.
- Sweating: Excessive perspiration without physical activity.
- Hunger: Sudden and intense feelings of hunger.
- Irritability or Mood Changes: Low glucose affects brain function, leading to mood swings.
- Confusion or Difficulty Concentrating: The brain lacks sufficient glucose to operate efficiently.
- Dizziness or Lightheadedness: Reduced blood sugar impacts overall stability.
- Rapid Heartbeat (Palpitations): The heart responds to adrenaline surges.
- Pale Skin: Blood vessels constrict in response to low glucose.
- Severe Symptoms: Seizures, loss of consciousness, or coma if not promptly addressed.
Onset and Progression:
- Rapid Development: Symptoms can appear suddenly.
- Immediate Risk: Hypoglycemia is acute and requires prompt treatment to prevent serious outcomes.
Key Differences
- Onset Speed:
- Hyperglycemia: Develops gradually.
- Hypoglycemia: Occurs suddenly.
- Symptom Nature:
- Hyperglycemia: Related to dehydration and the body’s attempt to eliminate excess sugar.
- Hypoglycemia: Due to adrenaline release and insufficient glucose supply to the brain.
- Energy Levels:
- Hyperglycemia: Fatigue from inefficient glucose utilization.
- Hypoglycemia: Sudden weakness or fatigue due to immediate energy deficiency.
- Hydration Status:
- Hyperglycemia: Causes dehydration (increased thirst and urination).
- Hypoglycemia: Does not typically affect hydration.
- Visual Symptoms:
- Hyperglycemia: Blurred vision from swollen eye lenses.
- Hypoglycemia: Visual disturbances from impaired brain function.
- Risk of Immediate Complications:
- Hyperglycemia: Long-term complications if unmanaged.
- Hypoglycemia: Immediate risk of seizures or loss of consciousness.
Recognizing these symptoms and understanding their differences is essential for timely and appropriate management. If you experience symptoms of either condition, it’s important to check your blood glucose levels and follow your healthcare provider’s recommendations.
How to Manage and Prevent Hyperglycemia and Hypoglycemia
Managing and preventing these conditions requires different strategies, but both hinge on maintaining stable blood sugar levels. For hyperglycemia, the goal is to reduce high blood sugar levels and prevent spikes. This involves monitoring blood sugar levels regularly, following a balanced diet with controlled carbohydrate intake, exercising regularly to improve insulin sensitivity, and adhering to a diabetes management plan, including taking medications as prescribed.
How to Manage and Prevent Hyperglycemia and Hypoglycemia
Understanding Hyperglycemia and Hypoglycemia
Hyperglycemia occurs when there is too much glucose in the bloodstream. It can be caused by insufficient insulin, overeating (especially carbohydrates), stress, illness, or lack of physical activity.
Hypoglycemia happens when blood glucose levels drop too low. This can result from taking too much insulin or other diabetes medications, skipping meals, excessive alcohol consumption, or increased physical activity without adequate food intake.
Managing and Preventing Hyperglycemia
- Monitor Blood Glucose Levels Regularly:
- Use a glucometer to check your blood sugar as recommended by your healthcare provider.
- Keep a log to track patterns and identify factors that affect your levels.
- Follow Your Meal Plan:
- Balanced Diet: Incorporate a mix of carbohydrates, proteins, and healthy fats.
- Carbohydrate Counting: Be mindful of carbohydrate intake, as it directly affects blood glucose.
- Portion Control: Avoid overeating by sticking to recommended serving sizes.
- Take Medications as Prescribed:
- Insulin Therapy: Administer insulin injections or use an insulin pump as directed.
- Oral Medications: Take pills at the same time each day to maintain consistent blood levels.
- Stay Physically Active:
- Engage in regular exercise like walking, cycling, or swimming.
- Consult your doctor before starting any new exercise regimen.
- Manage Stress:
- Practice relaxation techniques such as deep breathing, meditation, or yoga.
- Seek support from friends, family, or mental health professionals if needed.
- Stay Hydrated:
- Drink plenty of water to help your body eliminate excess glucose through urine.
- Regular Check-Ups:
- Visit your healthcare provider for routine examinations and lab tests.
- Adjust your treatment plan based on their recommendations.
Managing and Preventing Hypoglycemia
- Recognize Early Symptoms:
- Symptoms include shakiness, sweating, confusion, dizziness, and irritability.
- Treat immediately by consuming fast-acting carbohydrates.
- Carry Quick Sugar Sources:
- Keep glucose tablets, fruit juice, or hard candies accessible at all times.
- Eat Regular Meals and Snacks:
- Do not skip meals, especially if you’re taking insulin or glucose-lowering medications.
- Incorporate small snacks between meals if advised by your healthcare provider.
- Adjust Medication Dosages:
- Consult your doctor to modify insulin or medication doses if you’re experiencing frequent lows.
- Be Cautious with Alcohol:
- If you drink alcohol, do so with food and monitor your blood sugar levels closely.
- Plan for Physical Activity:
- Check your blood sugar before and after exercise.
- Consume a snack before exercising if levels are low.
- Educate Family and Friends:
- Teach those close to you how to recognize signs of hypoglycemia and how to assist.
General Tips
- Medical Identification: Wear a medical ID bracelet or carry a card that indicates you have diabetes.
- Emergency Plan: Have a plan in place for severe highs or lows, including emergency contacts.
- Stay Informed: Keep up-to-date with the latest diabetes management strategies.
- Consult Professionals: Work closely with your healthcare team, including doctors, dietitians, and diabetes educators.
This information is intended for general guidance and should not replace professional medical advice. Always consult your healthcare provider for personalized recommendations tailored to your specific condition.
Conclusion and the Importance of Seeking Medical Advice
Understanding the difference between symptoms of hyperglycemia and hypoglycemia is vital for anyone managing their blood sugar levels, especially for those with diabetes. Recognizing the signs early and knowing how to respond can prevent serious complications and improve the quality of life.
It’s also essential to seek medical advice if I’m consistently experiencing symptoms of either condition, as they may indicate the need for changes in my diabetes management plan or other health concerns. Regular check-ups with my healthcare provider can help detect potential problems early and allow for timely intervention.
In conclusion, while managing blood sugar levels can be challenging, staying informed, vigilant, and proactive in my approach to health can lead to successful management of both hyperglycemia and hypoglycemia. Remember, health is a journey, and I’m not alone in it—medical professionals are there to guide and support me every step of the way.
















[…] Regular blood glucose monitoring is crucial for individuals managing diabetes. By choosing the right blood glucose meter, you can ensure accurate and reliable results while keeping costs affordable. The ten best affordable blood glucose meters discussed in this article offer a range of features and benefits to suit different needs and preferences. […]